What is Candidiasis?
Candidiasis is an infection caused by a yeast called Candida. There are over 160 species of Candida, but only 20 of them cause disease in humans. Candida albicans is the most common.
The yeast Candida can naturally be found on the skin, in the mouth, on genital organs, or within the gastrointestinal tract of up to 80% of the population.
Under normal circumstances, the mere presence of Candida in our bodies does not pose any danger. Our immune system effectively controls the population of this fungus, allowing it to exist only in small amounts.
Problems with the Candida fungus arise when our immune system weakens or when there is a sudden change in the natural flora of bacteria on our skin, such as in cases of prolonged antibiotic use. These changes make our bodies more prone to Candida proliferation. The yeast begins to reproduce without limitations, potentially infesting the skin and invading deeper tissues, causing an intense inflammatory reaction.
Candidiasis is the term used to describe the infection caused by Candida. Having Candida on the skin asymptomatically is different from having the disease candidiasis. Colonization is not synonymous with infection.
Candidiasis has the potential to impact a variety of organs, most commonly affecting the skin, genitals, and mouth. In more extreme instances, typically involving patients who suffer from significant immunosuppression, Candida can invade internal organs like the esophagus, larynx, kidneys, heart, and even the central nervous system.
This article will discuss only thrush in men (yeast infection on the penis), which manifests as an infection of the glans or foreskin, referred to as balanitis or balanoposthitis, respectively.
What is Candida Balanitis or Balanoposthitis?
Balanitis and balanoposthitis are terms often treated as synonyms. However, there is a slight difference.
Balanitis is the name given to any inflammation of the glans, popularly known as the head of the penis. When the foreskin, the skin covering the glans, is also inflamed, the condition is known as balanoposthitis.
In uncircumcised men, inflammation of the glans is almost always accompanied by inflammation of the foreskin. In circumcised men, the absence of the foreskin means that only balanitis is possible.
From this point forward, to simplify the explanation, I will use only the term balanitis, as it encompasses both circumcised and uncircumcised men.
Candida balanitis is the most common penile infection, accounting for 25 to 50% of balanitis cases. Despite being the most common cause of penile infection, Candida balanitis is about ten times less common than vaginal infection caused by Candida.
The fundamental prerequisite for the development of Candida balanitis is the colonization of the penis by Candida. It is estimated that around 20 to 25% of men experience yeast colonization on their penises. However, not all of them will develop an infection; in fact, nearly two-thirds continue to be asymptomatic carriers throughout their lives.
How do Men Get Yeast Infections?
In adult men, the primary source of yeast colonization is unprotected sexual activity. If a woman’s vagina has large populations of Candida, during intercourse, a significant amount of the fungus can be transferred to the penis, increasing the risk of balanitis.
However, not all cases of male urogenital candidiasis originate from sexual activity. Babies and children can also experience fungal balanitis. In pediatric patients, acquiring Candida albicans is related to skin cleansing conditions and is often associated with diaper dermatitis. Moreover, Candida infection frequently correlates with antibiotic use (antibiotics reduce the population of skin bacteria, which are germs that compete for nutrients with fungi).
Risk Factors for Candida Balanitis
The development of penile candidiasis in colonized patients depends on the immune system’s ability to handle the large population of fungi living on the skin. Therefore, the mere presence of Candida in the genitals is insufficient; the fungus must have the freedom to multiply.
Balanitis has a wide variety of causes, but most cases are related to inadequate hygiene in uncircumcised men. When the foreskin is not routinely retracted, and the glans is not properly cleaned, there can be a buildup of sweat, debris, and dead skin, creating an environment highly favorable to fungal proliferation and inflammation.
Unsurprisingly, the risk of Candida balanitis is lower in circumcised men (Suggested reading: Circumcision: Risks, Benefits and Postoperative Care).
In addition to poor penis hygiene, other factors increase the risk of penile candidiasis, including:
- Use of glucocorticoids or other immunosuppressive drugs.
- Diabetes mellitus.
- Sexual partners with multiple episodes of vaginal candidiasis.
- Diaper use (in children or elderly).
- Recent antibiotic use.
- Immunosuppressive diseases, such as HIV.
- Chemotherapy.
- Malnutrition.
- Obesity.
- Illicit drug use.
- Edematous states (congestive heart failure, liver cirrhosis, or nephrotic syndrome).
Symptoms
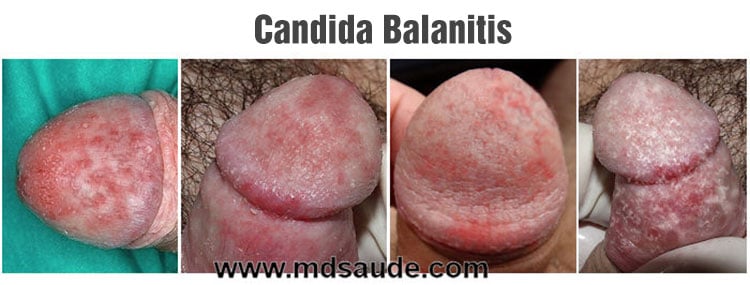
Candida infection in the penis typically presents as balanitis or balanoposthitis. The most common symptoms of male candidiasis include redness, swelling, itching, and pain in the glans. Additionally, white patches similar to those in oral candidiasis may appear on the penis.
These lesions can cause itching and often a burning sensation following sexual intercourse. The emergence of small blisters, ulcers, sores, skin peeling, or purulent discharge from the urethra is also frequent.
In uncircumcised patients, a thick and foul-smelling discharge may be present under the foreskin.
In summary, the symptoms of male candidiasis are:
- Burning and itching around the penis head, worsening after intercourse.
- Redness and swelling of the glans.
- Small reddish papules on the glans.
- Pain during urination.
- White patches around the glans.
- Thick, irregular discharge under the foreskin.
- Unpleasant odor in the foreskin.
- Difficulty retracting the foreskin.
Untreated Candida balanitis and balanoposthitis can lead to complications like phimosis or paraphimosis due to scarring, which makes the foreskin tighter and less retractable.
A diagnosis of candidiasis can be confirmed by scraping a small sample from the lesion and examining it under a microscope to identify Candida yeast.
Treatment
Antifungal creams or ointments can be used to treat candidiasis in men. The most effective treatment options for penile candidiasis include:
- Clotrimazole cream 1%, applied twice daily for 1 to 3 weeks
- Miconazole cream 2%, applied twice daily for 1 to 3 weeks
- Miconazole and hydrocortisone cream 1%, applied twice daily for 2 to 5 weeks
- Nystatin cream 100,000 IU/g, applied once or twice daily for 1 to 3 weeks
A simpler option is a single dose of oral fluconazole 150 mg.
For more severe cases, the best options are miconazole + hydrocortisone 1% cream or a fluconazole tablet.
In some instances, penile candidiasis may be an early symptom of developing diabetes mellitus. If a patient has no apparent risk factors for candidiasis, they should undergo a blood glucose evaluation.
Female sexual partners of men with Candida balanitis should be tested for candidiasis or may opt for empirical treatment to reduce the likelihood of reinfection.
If a patient experiences recurrent balanitis, circumcision may be considered as an option to reduce episodes.
Consuming yogurt containing lactobacillus may help decrease Candida colonization. Although no specific studies exist for lactobacillus in treating or preventing Candida balanitis, research showing a decrease in Candida colonization in the rectum and vagina provides a theoretical basis for its usefulness. While it may not work, it is unlikely to cause harm.
Alternative therapies with phytogenic agents, such as garlic, calendula, apple cider vinegar or chamomile sitz baths, pennyroyal tea, oregano oil, or goldenseal (Hydrastis canadensis), lack reliable data demonstrating their efficacy.
Frequently Asked Question
How long does it take for male candidiasis to clear up?
With appropriate treatment, patients generally experience significant symptom improvement within about seven days.
Can penile candidiasis improve on its own without treatment?
In milder cases, it can improve on its own. However, without treatment, recurrence is quite common.
Can candidiasis return after treatment?
Yes, approximately 10% of patients experience recurrent penile candidiasis despite receiving appropriate treatment.
What home remedies are effective for treating candidiasis in men?
No home remedies have been proven effective in controlled clinical studies.
Can Candida balanitis be transmitted to women?
Candida can be sexually transmitted. However, whether a woman subsequently develops Candida vaginitis depends on specific factors for each patient.
Should a man’s sexual partner be treated if he develops Candida balanitis?
While not mandatory, treating the partner can help prevent infection in women and reduce the likelihood of recurrences in men.
Can natural yogurt treat candidiasis in men?
Yogurt containing lactobacillus may help reduce Candida colonization. Still, it is unlikely sufficient for curing an infection on its own.
What is the best cream for penile candidiasis?
The most suitable creams for penile candidiasis are clotrimazole 1% or miconazole 2%. Another option is nystatin 100,000 IU/g.
What should be done if the cream does not resolve the issue?
If topical treatment is ineffective, a single 150 mg fluconazole tablet should be taken as an alternative treatment option.
References
- Balanitis in adults – UpToDate.
- Balanitis and balanoposthitis in children and adolescents: Clinical manifestations, evaluation, and diagnosis – UpToDate.
- Yeast infection in men: How can I tell if I have one? – Mayo Clinic.
- Genital colonisation and infection with candida in heterosexual and homosexual males – Genitourinary medicine.
- Candida balanitis: risk factors – Journal of the European Academy of Dermatology and Venereology.
- Mycotic infections of the penis – Andrologia.
- Balanoposthitis – Medscape.
- Candida Infections of the Genitourinary Tract – Clinical microbiology reviews.
Author(s)
Pedro Pinheiro holds a medical degree from the Federal University of Rio de Janeiro (UFRJ) and is a specialist in Internal Medicine and Nephrology, certified by the State University of Rio de Janeiro (UERJ) and the Brazilian Society of Nephrology (SBN). He is currently based in Lisbon, Portugal, with his credentials recognized by the University of Porto and the Portuguese Nephrology Specialty College.













Leave a Comment