What is Tinnitus?
Tinnitus is the term doctors use when a person experiences a buzzing, ringing, whistling, roaring, or other noise in one or both ears.
More specifically, tinnitus can be described as the perception of sound close to the head in the absence of any real external source. The sound may be perceived as being inside the ear(s), inside or around the head, or as a distant external sound.
Tinnitus is a common complaint with a prevalence of 10 to 20% of the population. The symptom may be short-lived or persist for months to years; it may be intermittent or continuous.
Tinnitus can be quite bothersome, to the point of interfering with a patient’s quality of life. In most cases, however, it is not a sign of a serious health problem, such as a malignant tumor or degenerative neurological disease.
Tinnitus can occur in children and becomes more common with age. It is more frequent in men than women, and is more likely to occur in people who smoke or frequently consume alcohol.
Causes
Tinnitus is usually caused by an underlying condition, inside or outside the ear, that causes the central nervous system to receive non-existent sound electrical signals. When tinnitus occurs without an apparent cause, it is called idiopathic tinnitus.
Almost everyone has experienced tinnitus briefly after exposure to extremely loud noises. For example, spending hours in a nightclub or being near a loud noise, such as a gunshot, can cause temporary tinnitus.
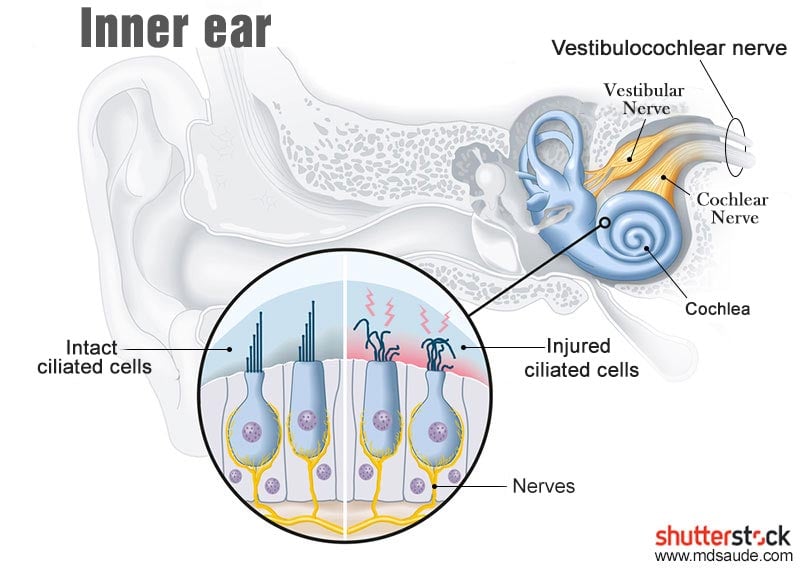
Persistent tinnitus, on the other hand, often occurs in people with damage to the inner ear, especially in the cochlea. In these cases, hearing loss is typically also present.
Inside the cochlea are tiny, delicate hair cells, called the cilia, that move when the ear receives sound waves. This slight movement triggers electrical signals along the cochlear nerve, which runs from the ear to the brain. When the brain receives these electrical impulses, it interprets them as sounds.
If the tiny hairs in your inner ear become bent or damaged – which can happen with age or regular exposure to loud noises – they can send random electrical impulses to your brain, resulting in tinnitus.
There are dozens of causes of tinnitus, most of which involve damage to the auditory pathways. The most common are listed below.
Presbycusis (Age-related Hearing Loss)
Hearing often deteriorates with age, especially after the age of 60. This form of hearing loss is usually bilateral and involves the sensory loss of high-frequency sounds.
Sensorineural hearing loss with aging partly explains why tinnitus is so common among older adults.
Noise-induced Hearing Loss
Exposure to loud noise, whether from a single traumatic experience or over months or years, can damage the auditory system and result in hearing loss and tinnitus.
Traumatic noise exposure can occur through contact with noisy machinery, music concerts, nightclubs, explosions, firearms, listening to loud music through headphones for extended periods, and so on.
Medications
Tinnitus can be triggered by ototoxic (ear-damaging) medications. Some examples of drugs that can cause or worsen tinnitus include:
- Acetylsalicylic Acid (ASA).
- Valproic Acid.
- Aminoglycoside antibiotics (streptomycin, gentamicin, amikacin).
- Fluoroquinolone antibiotics (ciprofloxacin, levofloxacin, moxifloxacin).
- Tricyclic antidepressants (amitriptyline, nortriptyline).
- Calcium channel blocker antihypertensives.
- Angiotensin-converting enzyme (ACE) inhibitors (captopril, enalapril, ramipril, lisinopril, perindopril).
- COX-2 inhibitor anti-inflammatories (Celecoxib, Arcoxia, Lumiracoxib).
- Antimalarials (chloroquine, hydroxychloroquine).
- Benzodiazepines (diazepam, alprazolam, lorazepam, oxazolam, midazolam, clonazepam).
- Carbamazepine.
- Cyclobenzaprine.
- Cisplatin.
- Clarithromycin.
- Chlordiazepoxide.
- Dapsone.
- Doxazosin.
- Furosemide.
- Proton pump inhibitors (omeprazole, esomeprazole, pantoprazole, lansoprazole).
- Isotretinoin.
- Prazosin.
- Quinidine.
- Sertraline.
- Sibutramine.
- Tolbutamide.
Drug-induced ototoxicity usually affects both ears, resulting in cochlear damage.
Ear Infection or Ear Canal Blockage
Accumulation of fluid, pus, wax, dirt, or other foreign matter can block the ear canal. Blockage of the auditory canal can change the pressure in the inner ear, causing cochlear dysfunction and tinnitus.
Otosclerosis
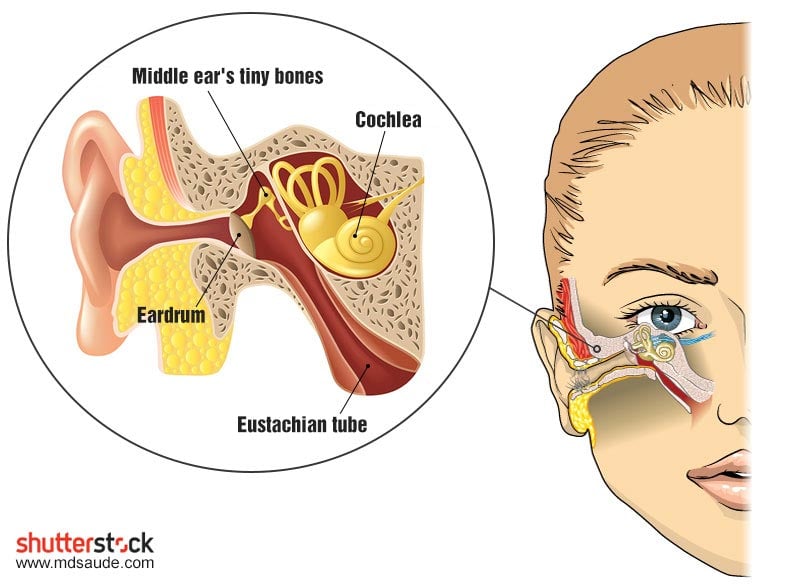
Our ear contains the three smallest bones in the human body: hammer (malleus), anvil (incus), and stirrup (stapes). Their purpose is to transfer the mechanical vibrations produced in the eardrum to the inner ear.
The hardening of the ossicles in the middle ear is called otosclerosis. Tinnitus can occur when otosclerosis damages the cochlear structures.
Progressive otosclerosis typically causes hearing loss, which may be unilateral or bilateral.
Eustachian Tube Dysfunction
The Eustachian tube, also known as the auditory tube, is a tube that connects the middle ear to the nasopharynx, allowing the air pressure on both sides of the eardrum to balance.
Patulous Eustachian tube is a disorder in which the Eustachian tube, which normally remains closed, is continuously open.
A patulous Eustachian tube can cause unilateral or bilateral tinnitus, with sounds similar to ocean noise, typically synchronized with breathing. Unusual perception of one’s own voice (autophony) and ear discomfort are also common. The symptoms usually disappear when the patient lies down.
Acoustic Neuroma or Other Head and Neck Tumors
An acoustic neuroma is a benign tumor that compresses the vestibulocochlear nerve, which is responsible for balance and hearing. Other head, neck, or brain tumors can also cause tinnitus, which is usually unilateral.
Vascular Diseases
Conditions affecting the blood vessels around the ear and the temporal bone, such as atherosclerosis, high blood pressure, or twisted or malformed blood vessels, can cause changes in blood flow, leading to the appearance of a pulsatile tinnitus.
Neurological Causes
Tinnitus can result from the spasm of one or both muscles of the middle ear (the tensor tympani muscle and the stapedius muscle), which are innervated by cranial nerves.
These muscular spasms can occur spontaneously due to disease of the ear itself or some neurological disease, such as multiple sclerosis.
Noises with the sound of clicking or irregular or rapid pulsations can also result from the myoclonus of the muscles in the palate area (roof of the mouth), which attach to the opening of the Eustachian tube.
Palatal muscle myoclonus is typically caused by a neurological abnormality, such as multiple sclerosis, microvascular disease of the brain stem, or neuropathy related to metabolic changes or intoxications.
Risk Factors
Anyone can develop tinnitus, but those who exhibit one or more of the factors listed below are at a higher risk:
- Loud noise exposure.
- Advanced age.
- Being male.
- Smoking.
- Alcohol consumption.
- Obesity.
- Diabetes mellitus.
- High cholesterol.
- High blood pressure.
- Head trauma.
- Sleep deprivation (less than 6 hours per night).
- Depression.
- Anxiety.
- Thyroid diseases.
- Ear infection.
- Rheumatoid arthritis.
- Ménière’s disease.
Types of Tinnitus
Tinnitus can be classified in various ways according to its characteristics. The main ones are:
Subjective Tinnitus: These are noises in the head or ears that are only perceptible to the patient. Subjective tinnitus usually arises in people with hearing loss. Over 99% of all reported tinnitus cases are subjective.
Objective Tinnitus: These are noises in the head or in one ear that are audible to the patient and other people. These sounds, usually pulsatile, are produced by vascular changes around the ears or by muscle spasms in the same region. Objective tinnitus is rare, representing less than 1% of total tinnitus cases.
Pulsatile Tinnitus: These are noises described as regular pulsation sounds. Pulsatile tinnitus can be either subjective or objective.
Primary Tinnitus: This is idiopathic tinnitus, which arises without any apparent cause and may or may not be associated with sensorineural hearing loss, a type of hearing loss where the root of the problem lies in the inner ear or sensory organ (cochlea and associated structures) or the vestibulocochlear nerve (eighth cranial nerve). Sensorineural hearing loss is responsible for about 90% of the causes of deafness.
Secondary Tinnitus: Tinnitus associated with a specific underlying cause, apart from sensorineural hearing loss
Acute Tinnitus: Any tinnitus that has been present for less than six months.
Chronic Tinnitus: Any tinnitus present for more than six months.
Diagnosis
When a patient complains of tinnitus, the doctor should attempt to identify the origin of the symptom. The most suitable specialist to conduct this investigation is the otolaryngologist.
Tinnitus is often associated with hearing loss or some other cochlear injury. In some cases, tinnitus may be the initial complaint in a patient with central nervous system damage.
History taking and physical examination are the first steps in establishing the origin of tinnitus. An audiometry test to detect if there is hearing loss should be performed, especially in those with unilateral tinnitus. An evaluation of the eardrum through otoscopy should also always be carried out.
During the patient’s clinical assessment, it’s crucial to identify the characteristics of the tinnitus, whether it is episodic or constant, pulsatile or non-pulsatile, its rhythmicity, high or low pitch, sound quality, etc.
Patients should also be asked about known ear diseases, exposure to noise, history of head trauma, and associated symptoms, such as hearing loss and dizziness.
All medications and supplements should be reviewed. The history should revisit other medical conditions, including high blood pressure, atherosclerosis, neurological disease, and previous surgeries.
Patients should be questioned explicitly about depression, anxiety, and insomnia, which can exacerbate tinnitus and increase its impact on quality of life.
Tinnitus that is clearly pulsatile and that increases in intensity with exercise is usually of vascular origin. Changes in the intensity of tinnitus with head movement or changes in body position (lying down versus sitting or standing) also strongly suggest vascular tinnitus.
In patients with suspected vascular tinnitus, the doctor should auscultate the neck regions, the area around the ears, temples, and around the orbit, ideally in various positions to see if there is a change in the tinnitus pattern.
Tinnitus with a clicking sound is often related to muscle problems. Myoclonus of the palatine muscles or the middle ear structures can occur spontaneously, but it may also suggest some significant neurological disease.
When there is suspicion of intracranial vascular injury, magnetic resonance imaging or computed tomography should be requested.
Treatment
Tinnitus treatment involves the rectification of identified conditions, as well as directly addressing the effects of tinnitus on the patient’s quality of life.
All risk factors and identified causes should be treated. This includes discontinuation of medications that may be causing the tinnitus, treatment of depression or insomnia, cessation of alcohol and tobacco, removal of possible earwax plugs, surgical correction of vascular lesions, use of hearing aids or cochlear implants for those with some degree of deafness, etc.
In many cases, treating the conditions described above is sufficient to improve the patient’s tinnitus significantly.
However, tinnitus is a chronic condition without a correct cause for many. This is particularly true for patients with sensorineural hearing loss. In these individuals, the primary goal of treatment should be to reduce the impact of the noises on the patient’s life.
Masking
There are treatments that can help make tinnitus less noticeable. Masking devices resemble hearing aids and are designed to produce low-level sounds that reduce the perception of tinnitus.
The otolaryngologist may suggest using these electronic devices to suppress tinnitus, such as hearing aids that produce so-called “white noise”, which are constant, monotonous sounds, similar to those of a TV off-air or a machine on, or environmental sounds like rain or ocean waves.
Fans, humidifiers, dehumidifiers, and air conditioning in the bedroom also produce white noise and can help make tinnitus less noticeable at night.
TRT
Tinnitus Retraining Therapy (TRT), like masking, is a treatment technique for tinnitus that also utilizes habituation and sound therapy to help individuals manage tinnitus symptoms. TRT aims to assist the brain in adapting to tinnitus, making it less noticeable and disruptive.
TRT is a more comprehensive therapy that combines masking with cognitive-behavioral therapy to help patients cope with the emotional impact of tinnitus and reprogram the patient’s brain to interpret tinnitus as a less intrusive and distressing sound.
TRT therapy involves using custom sound amplification devices (usually hearing aids) and sound therapy to help patients get accustomed to tinnitus. The sound amplification devices are adjusted to provide a gentle, constant background sound for a specific period to reduce the perception of tinnitus.
Over time, TRT helps reprogram the patient’s brain to interpret tinnitus as a less intrusive and distressing sound. This can help patients feel more comfortable and cope better with tinnitus, allowing them to focus on other activities and daily tasks.
TRT is considered an effective treatment for tinnitus in many cases. However, it may take time for patients to begin seeing significant results, and TRT therapy generally requires multiple sessions and adjustments over time to be effective. TRT treatment may take one to two years until the patient no longer needs the device.
Electrical Stimulation
Electrical stimulation of the cochlea through direct electrode placement appears to result in tinnitus improvement in patients with hearing loss. Transcutaneous electrical stimulation is the only available electrical option not associated with the risk of causing hearing loss.
Electrical stimulation can be provided via a single electrode or through acupuncture needles placed several times over the mastoids or around the auricle.
However, external electrical stimulation to the middle or inner ear has not been proven more effective for tinnitus suppression than placebo treatment in patients without hearing loss.
Pharmacological Treatments for Tinnitus
There are no medications that directly treat tinnitus. Generally, drugs that show some response are those used to treat underlying issues, such as depression, anxiety, or insomnia.
Any medication or supplement sold as an effective treatment for tinnitus, especially those marketed outside of pharmacies, is misleading advertising. Currently, there is no cure for tinnitus.
Gamma-Aminobutyric Acid (GABA)
Gamma-aminobutyric acid (GABA) is a neurotransmitter that plays a significant role in regulating the central nervous system. Although GABA is known for its relaxing and inhibitory properties on the central nervous system, there is scant scientific evidence to support its use in treating tinnitus.
Some preliminary studies suggest that GABA might effectively reduce tinnitus symptoms in some people, but current evidence is limited and inconclusive. The main research on the subject was conducted on rats and with drugs toxic to humans.
It’s important to note that most GABA supplements sold on the internet are poorly absorbed by the body when taken orally, as GABA cannot readily cross the blood-brain barrier, a protective membrane that restricts the entry of substances from the blood into the brain.
If you take GABA supplements, it will not affect tinnitus, as the substance does not reach the brain regions where it could act to reduce the ringing.
While there are some drugs containing compounds related to GABA that can reach the brain and may have similar effects to GABA in the body, these compounds have severe side effects, and their use should be monitored by a healthcare professional.
In summary, although GABA may hold promise for treating tinnitus in some cases, current evidence is limited and inconclusive. The options that could be effective are complex and carry a high risk of side effects. At present, the benefits clearly do not outweigh the risks.
Other Tinnitus Treatments Lacking Scientific Evidence
Whenever a common disease lacks an effective treatment, dozens of “alternative, natural, or home remedies” emerge to fill that gap. However, many of these have yet to be studied or have not shown positive results in clinical trials. Here are a few examples:
- Acupuncture: studies have found acupuncture no more effective than placebo.
- Zinc: studies correlating zinc levels with tinnitus and randomized, controlled trials of zinc therapy for tinnitus have yielded inconsistent results. Current evidence does not support the use of zinc supplements for tinnitus treatment.
- Ginkgo biloba: ginkgo biloba and other bioflavonoids have been promoted as tinnitus-reducing substances, but there is no evidence of their efficacy.
- Anticonvulsants: anticonvulsants do not appear to be effective in improving non-pulsatile tinnitus symptoms. A systematic review and meta-analysis that included seven randomized trials of patients with chronic tinnitus found no clinically significant effect on symptoms when comparing anticonvulsants (gabapentin, carbamazepine, lamotrigine, and flunarizine) with placebo. However, carbamazepine appears to have some efficacy in treating pulsatile tinnitus.
- Melatonin: controlled studies have not found melatonin to be effective for tinnitus.
- Vitamins: no type of vitamin, including niacin (vitamin B3), has proven effective for tinnitus in controlled studies.
References
- Clinical Practice Guideline: Tinnitus – American Academy of Otolaryngology – Head and Neck Surgery.
- Tinnitus – The Lancet.
- Etiology and diagnosis of tinnitus – UpToDate.
- Treatment of tinnitus – UpToDate.
- Tinnitus – Medscape.
- Tinnitus – American Tinnitus Association.
- Underlying Mechanisms of Tinnitus: Review and Clinical Implications – Journal of the American Academy of Audiology.
- A review of tinnitus – The Royal Australian College of General Practitioners.
- Flint PW, et al., eds. Tinnitus and hyperacusis. In: Cummings Otolaryngology: Head and Neck Surgery. 7th ed. Elsevier; 2021.
Author(s)
Pedro Pinheiro holds a medical degree from the Federal University of Rio de Janeiro (UFRJ) and is a specialist in Internal Medicine and Nephrology, certified by the State University of Rio de Janeiro (UERJ) and the Brazilian Society of Nephrology (SBN). He is currently based in Lisbon, Portugal, with his credentials recognized by the University of Porto and the Portuguese Nephrology Specialty College.


Leave a Comment