Introduction
Nursing women can produce sufficient amounts of breast milk, in both quantity and quality, for their babies, even when they are not consuming adequate nutrition. During breastfeeding, the female body gives priority to milk production. But there are limits to how much the body can compensate for an inadequate diet in terms of quality or quantity of calories and nutrients.
However, just because your baby may not be adversely affected by occasional lapses in your diet doesn’t mean that you won’t face nutritional issues. When a breastfeeding woman has a problematic diet and cannot obtain the necessary nutrients, her body will tap into its reserves, which may eventually deplete.
Adopting restrictive diets for weight loss during breastfeeding is not recommended, as the mother needs strength and stamina to produce milk and care for the baby.
Maternal weight during lactation
Weight changes in breastfeeding women vary greatly. Typically, gradual weight loss occurs during the first six months of breastfeeding.
This weight loss may be greater or lesser depending on factors such as the quality and quantity of food intake, physical activity, weight gain during pregnancy, pre-pregnancy weight, muscle mass, maternal age, length of maternity leave, and more.
These factors can cause a difference in the rate of weight loss of up to 2.2 pounds (1 kilogram) per month between two breastfeeding women.
It is important to remember that during the first few weeks, much of the weight loss is due to the shedding of water retained during pregnancy. After the swelling subsides, weight loss occurs through the elimination of fat.
In well-nourished women, there is usually no significant loss of muscle mass during the lactation period. Weight loss occurs primarily through the consumption of adipose tissue (fat).
Although it is widely publicized that breastfeeding helps women lose weight after pregnancy, this relationship remains controversial. Different studies show conflicting results, ranging from greater weight loss with breastfeeding, to less weight loss with breastfeeding, to no difference in weight loss between breastfeeding and non-breastfeeding women.
It is a fact that milk production increases the mother’s basal caloric expenditure. A lactating woman must consume an average of 500 more calories to maintain adequate caloric daily intake. However, there is no need to worry about counting calories in your diet as most women tend to increase their caloric intake naturally due to the increased hunger that breastfeeding induces.
Fluid intake
On average, breastfeeding women produce about 750 to 800 ml of breast milk per day. Many women are unsure about how much water they should drink during the breastfeeding period to avoid interfering with milk production.
Quantifying the volume of fluids you drink throughout the day is unnecessary. The key is to drink enough water to avoid feeling thirsty, aiming to keep your urine consistently diluted and clear.
For convenience, keep a glass of water nearby before each breastfeeding session so that you can access it when you feel like drinking.
Avoid beverages with caffeine, as it can be passed to your baby through the milk, and caffeine is also a diuretic, which can lead to further dehydration.
Recommended Nutrients for Breastfeeding Women
In most cases, a mother’s regular diet is more than adequate to maintain good nutritional status for both herself and her baby. Increased hunger is an excellent mechanism for unconsciously raising the consumption of calories, proteins, and other nutrients to desirable levels.
The following are brief comments on some of the nutrients that are the source of the most confusion among lactating women.
Iron
On average, breast milk provides about 3 mg of iron per day. Generally, if the mother is not anemic, there is no need for iron supplementation; a balanced diet suffices.
Iron loss through breastfeeding is less than the usual iron loss during menstruation. Since women do not menstruate in the first few months of breastfeeding, they end up having better iron stores during breastfeeding than at other times in their lives.
Good sources of iron include meats, beans, peas, lentils, fortified cereals, whole-grain products, dark green leafy vegetables, and dried fruits. To aid absorption, try to consume iron-rich foods with vitamin C-rich foods, such as strawberries, citrus fruits, or tomatoes.
Proteins
The average amount of protein excreted daily in breast milk is 8 grams. Increasing the daily protein intake by 25 grams in the regular diet is recommended to compensate for these losses.
In general, the amount of protein in milk does not change even if the mother’s dietary protein intake is low. The problem of protein deficiency is not for the baby, but for the mother, who may begin to lose muscle mass.
Good protein sources include meat, eggs, dairy products, soy, legumes, lentils, nuts, seeds, and whole grains.
Calcium
About 210 mg of calcium is excreted in breast milk daily. Breastfeeding can cause a temporary reduction in the amount of calcium in the bones.
Studies indicate that this loss cannot be reversed, even with an increase in dietary calcium. The good news is that this fact appears to have little clinical relevance, as bone loss is usually recovered after the breastfeeding period ends.
In addition, some studies suggest that older women who breastfed in their youth have a lower incidence of osteoporosis than women who did not breastfeed.
Therefore, there is no need to increase calcium intake during breastfeeding. All mothers should consume at least 1,000 mg of calcium daily, which is the amount recommended for all women in general.
The main sources of dietary calcium are milk and other dairy products, such as cheese, butter, and yogurt. Green vegetables, such as spinach, are also good choices.
Vitamins
Vitamins are also excreted in milk, so increasing your vitamin intake during breastfeeding is recommended.
Once again, a varied diet rich in fruits, vegetables, legumes, and meats is sufficient to meet these needs. If you cannot maintain a balanced diet, your doctor may recommend using multivitamins to ensure good intake of vitamins A, E, C, and B.
What the mother should not eat during breastfeeding?
Certain foods and beverages should be avoided or significantly reduced during breastfeeding. We will discuss some of these.
Alcohol
When a breastfeeding woman consumes alcohol, a small amount is passed into the breast milk. The amount of alcohol considered “safe” during breastfeeding is controversial. Several factors affect the amount of alcohol that passes into breast milk and how much of it is absorbed by the baby.
For a woman of average weight, it takes about two hours for a single dose of alcohol (a glass of beer or a glass of wine) to be completely metabolized and eliminated from the body.
Therefore, to avoid passing any amount of alcohol to the baby, experts recommend that women do not consume alcohol if they intend to breastfeed within the next 2 to 3 hours.
Please note that using a breast pump to express milk will not hasten the process of removing alcohol from the milk.
Caffeine
Most doctors recommend that mothers limit their caffeine intake (including coffee, tea, soda, energy drinks, chocolate, etc.) to no more than 200 to 300 mg per day (about two to three cups of coffee per day) while breastfeeding.
Note: This 300 mg limit is still under debate, so it is best to limit caffeinated foods as much as possible. If your baby becomes irritable due to caffeine in your diet, eliminate coffee, soda, and chocolate from your diet.
Chocolate
Chocolate contains small amounts of caffeine and larger amounts of a closely related compound, theobromine. It also contains anandamide and two related compounds that stimulate cannabinoid receptors: tryptophan and polyphenols.
All of these compounds can be found in small amounts in breast milk. A low intake of chocolate (1 bar per day) by a breastfeeding mother is not problematic, but a high intake may affect the baby.
Fish with high levels of mercury
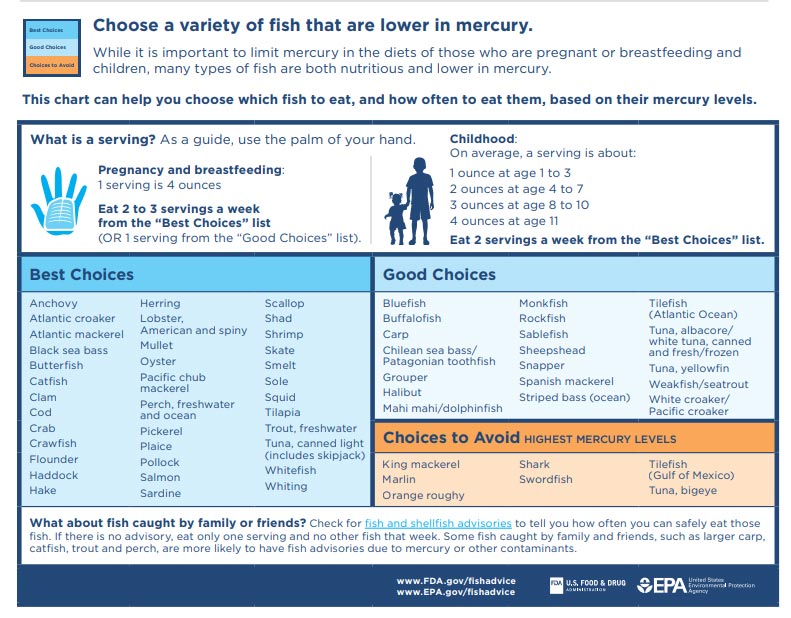
Fish provides high-quality protein and other essential nutrients, including omega-3 fatty acids. The consumption of fish by breastfeeding mothers has been suggested because of the high amount of essential fatty acids, which are critical to the newborn’s brain development.
However, almost all fish and shellfish contain traces of mercury. For most people, this small amount is irrelevant. However, even traces of mercury appear to be harmful to a baby’s developing nervous system.
Therefore, breastfeeding mothers should avoid eating fish known to be high in mercury. The most notable are:
- King mackerel (Scomberomorus cavalla).
- Marlin (family Istiophoridae).
- Orange roughy (Hoplostethus atlanticus).
- Shark
- Swordfish (Xiphias gladius).
- Tilefish (Gulf of Mexico)
- Bigeye Tuna.
The chart below is from the FDA and helps you choose which fish to eat.
Artificial Sweeteners
Saccharin, sucralose, and potassium acesulfame have been detected in human milk at low levels when consumed by breastfeeding mothers.
Maternal consumption of typical amounts is not likely to cause adverse effects in babies, although some experts advise against maternal consumption of large amounts of these substances.
Aspartame is not secreted in human breast milk, even when consumed in amounts much higher than typical, making it the safest option for the baby.
Sports Supplements for Breastfeeding Mothers
Creatine
Creatine is a dietary supplement to increase muscle mass and improve exercise performance. It is probably the most studied sports supplement with the best safety profile. However, there are no specific studies on breastfeeding mothers.
Creatine is a normal component of human milk, providing about 9% of a baby’s daily requirement. However, no study has measured creatine levels in human milk after supplementation.
Creatine is converted to creatinine in the mother’s and baby’s bodies. Maternal use of creatine supplements may increase the baby’s serum creatinine, altering estimates of the baby’s kidney function.
Some authors speculate that creatine supplementation in breastfeeding mothers may help prevent creatine deficiency syndromes, but no studies are available to test this hypothesis.
It is probably safe, but until more safety data are available, it is better to avoid creatine supplementation unless prescribed by a healthcare professional.
Whey Protein
Whey protein supplements are allowed and often recommended for breastfeeding mothers who cannot maintain adequate protein intake.
The only caveat is regarding the product’s quality. If you are going to take Whey, choose a high-quality brand with good-quality certificates to ensure there are no harmful substances, such as hormones, caffeine, or stimulants, hidden in its formula.
Babies who do not tolerate certain foods
Most mothers can eat a wide variety of foods, including spicy ones, without causing any reaction in their babies.
However, some foods are more associated with baby discomfort, causing gas, colic, and irritation. These include:
- Broccoli.
- Cabbage.
- Cow’s milk.
- Nuts.
- Eggs.
- Chocolate.
- Citrus fruits.
- Garlic.
- Bell pepper.
- Spicy foods.
- Soy.
- Seafood.
- Onion.
Mothers should understand that babies can have good and bad days without any apparent reason. It’s common for mothers to blame their diet for any changes in their baby’s behavior, but it may not always be the case.
When a baby experiences colic, it’s natural to assume that the mother’s recent consumption of eggs, milk, or spicy food may have caused it. However, it’s important to remember that just because these events occurred together, it doesn’t necessarily mean one caused the other. Correlation does not necessarily imply causation. While the mother’s diet could be a factor, it’s not always the sole cause of colic. Other reasons should also be considered.
However, if you suspect that a particular food is making your baby more fussy than usual, it might be a good idea to eliminate it for a few days and see if there’s a response. But be aware that even if your baby’s mood improves, it doesn’t prove that the food is to blame. As we said, a baby’s mood can vary significantly from day to day during the first few months of life.
In rare cases, your baby may be allergic to something you have eaten. In these cases, you may notice skin reactions, noisy breathing, nasal congestion, and changes in the usual characteristics of the stool. If you suspect an allergy, contact your pediatrician.
Frequently Asked Questions
Can a mother’s diet influence the taste of breast milk?
Absolutely. A mother’s diet has the ability to subtly alter the flavor of breast milk, introducing the baby to a variety of tastes that can help with the transition to solid foods in the future.
Should a nursing mother consume more calories during the breastfeeding period?
Yes, increasing calorie intake during lactation is generally recommended to compensate for the energy expended in milk production.
What should I eat during breastfeeding to prevent colic in my baby?
Baby colic is not necessarily related to the mother’s diet. However, some foods may irritate the baby. If your baby is frequently colicky, you can keep a meal diary, noting what you ate, to identify any food that may be exacerbating the situation.
I’m breastfeeding; can I drink coffee?
Caffeine does pass into breast milk, but one or two cups of coffee daily are usually not harmful. More than three may be excessive.
It is important to note that some babies are more sensitive to caffeine and can become irritable or have difficulty sleeping, even with small amounts of caffeine.
Babies’ sensitivity typically decreases over time as their ability to metabolize caffeine improves with growth, reaching levels similar to adults by five months.
Can I eat chocolate while breastfeeding?
Yes. In moderate amounts, such as a bar of chocolate per day, there is no evidence of harm to the baby.
How long should I wait to breastfeed after drinking alcohol?
Ideally, you should not drink alcohol. But if it has already happened, it is safest to wait at least two to three hours if you have had a glass of beer or wine.
Does beer increase milk production?
No, this is a myth. No alcoholic beverages stimulate milk production. The same is valid for non-alcoholic beer.
What should I eat to help with milk production?
Proteins, calories, and water.
References
- Maternal nutrition during lactation – UpToDate.
- Creatine – Drugs and Lactation Database (LactMed®) – National Library of Medicine – NIH.
- Chocolate – Drugs and Lactation Database (LactMed®) – National Library of Medicine – NIH.
- Macronutrient and Micronutrient Intake during Pregnancy: An Overview of Recent Evidence – Nutrients.
- Pregnancy Nutrition – American Pregnancy Association.
- Prenatal and Postnatal Flavor Learning by Human Infants – Pediatrics.
- Advice about eating fish – For those who might become or are pregnant or breastfeeding and children ages 1 – 11 years – FDA.
- Lawrence RA, et al. Maternal nutrition and supplements for mother and infant. In: Breastfeeding: A Guide for the Medical Profession. 8th ed. Elsevier; 2016.
- Hetzel Campbell S, et al. Nutrition during lactation. In: Core Curriculum for Interdisciplinary Lactation Care. Jones & Bartlett Learning. 2019.
Author(s)
Pedro Pinheiro holds a medical degree from the Federal University of Rio de Janeiro (UFRJ) and is a specialist in Internal Medicine and Nephrology, certified by the State University of Rio de Janeiro (UERJ) and the Brazilian Society of Nephrology (SBN). He is currently based in Lisbon, Portugal, with his credentials recognized by the University of Porto and the Portuguese Nephrology Specialty College.





Leave a Comment